AAI interviewed member Marianne Gontarz York, M.S.W, L.C.S.W., gerontologist and photographer. Marianne is a renaissance woman, with a passionate, thoughtful and insightful understanding of the mental health and aging landscape in Marin. She talks about becoming an advocate for older adults and being a part of the AAI Mental Health and Dementia workgroup. Her award-winning black and white photos are featured throughout.
 What is Mental Health? Dementia?
What is Mental Health? Dementia?
There is curiously no straightforward definition of mental health. We can better define the absence of mental health: a mental illness or a disturbance. I consider mental health good brain health. When it comes to illness and disturbance, the American Psychiatric Association (APA) is the ultimate definer.
Disturbances in mental health are classified into a system based on the APA Diagnostic and Statistical Manual of Mental Disorders, commonly referred to as DSM-V. Disturbances that are often associated with aging are: Dementia, Delirium, Amnesic and other cognitive disorders now called Major Neurocognitive Disorders, Depressive Disorders, Anxiety Disorders and Substance-related Disorders.
Depression and Anxiety Disorders are disorders affecting a person’s mood and are considered treatable with a combo of drugs and Talk therapy. Alzheimer’s Disease and its related disorders (vascular dementia, Lewy Body dementia, et al.) are organic in nature, degenerative and not considered treatable at this point in time.
Someone can have a combination of both. For example, someone who is diagnosed with Alzheimer’s disease can become depressed and/or anxious.
Someone with any recently diagnosed medical condition (heart disease, cancer, etc.) can become depressed and/or anxious as well.
Additionally, sometimes depression and dementia share the same symptoms.
The CDC estimates that 20% of people 55 plus experience some type of mental health concern. The most common conditions include mood disorders, anxiety and/or depression, and cognitive impairment.
How are you involved?
I have worked in both areas of mental health throughout my nearly four-decade career. I have directed both mental health and Alzheimer’s adult day health and day care programs. Three years ago, I was appointed as a Commissioner to the Commission on Aging (COA).
I was also recently appointed to the Mental Health Services Act (MHSA) Advisory Committee and, with the Commission’s support, I am eager to have a positive impact. For the past four years, the COA has been working hard to get some attention for mental health programs. MHSA has released a draft of its Three-Year Program and Expenditure Plan and the Commission on Aging has written its response. I am proud of the advocacy work we have been doing in this area. To read the COA response to the MHSA draft plan, click here.
 How did you get into this kind of work?
How did you get into this kind of work?
I grew up in the city of Boston. I joined VISTA after I graduated from Boston University with a B.A. I studied Social Work with a focus on gerontology. I was assigned to relocate people who had been tenants in rooming houses. The majority of people being displaced were old and poor and women. They didn’t want to leave their neighborhood. I advocated to the housing authorities as hard as I knew how so that these older people could be relocated within their neighborhood.
Sometimes I got lucky and people got to return to a renovated apartment in their old building. One woman who I will never forget, Cora Moreau, was forced to move out of her neighborhood. Her new living room window faced a cemetery. She became quite depressed. This didn’t seem right or fair. You could say that my awareness of some of the challenges facing older adults, as well as mental health issues was birthed there.
 I realized that I liked working with older people and that I needed to get better credentials if I were to have an impact as an advocate for older people, so I decided to go to graduate school. It was there that I had the good fortune to meet Dr. Louis Lowy. He developed the gerontology program at Boston University’s School of Social Work.
I realized that I liked working with older people and that I needed to get better credentials if I were to have an impact as an advocate for older people, so I decided to go to graduate school. It was there that I had the good fortune to meet Dr. Louis Lowy. He developed the gerontology program at Boston University’s School of Social Work.
Dr. Lowy foresaw the coming “Age Wave” and knew that we as a culture weren’t prepared for it. He encouraged us, his students, to challenge our culture’s negative beliefs about aging. Retirement and its issues were the focus of my interest in graduate school. With life expectancy increasing, retirement was a period that could last 25 to 30 years!
Dr. Lowy was an Auschwitz survivor; he advocated that you had to impose meaning on life to make it worthwhile. He found his meaning in the field of aging. He savored every day of his life and knew that he was lucky to grow old. In the preface to his book Social Work with the Aged (1979) he wrote, “With more and more people living beyond 65 years of age, the question arises: FOR WHAT PURPOSE?”
 Shortly after graduate school (1979) I received a summer fellowship grant to the Maine Photographic Workshops. It was then that I discovered the work of Dorothea Lange. Lange’s photographs were used to advocate for change (in the 1930s and 1940s). Lange believed that the camera teaches people to see their world – for many, the world is a blur. She was an informed photographer, and her goal was to influence the way people thought.
Shortly after graduate school (1979) I received a summer fellowship grant to the Maine Photographic Workshops. It was then that I discovered the work of Dorothea Lange. Lange’s photographs were used to advocate for change (in the 1930s and 1940s). Lange believed that the camera teaches people to see their world – for many, the world is a blur. She was an informed photographer, and her goal was to influence the way people thought.
Likewise, I set out as a social worker and photographer with the question: How do older people find meaning and fulfillment in this period we call “retirement”? I wanted to find answers and then influence the way people – specifically “Baby Boomers” – thought about aging.
Back from my summer in Maine, I met Jim Callahan, PhD, a well-respected gerontologist affiliated with Brandeis University. He alternated between being a public servant, Massachusetts’s Secretary of Elder Affairs and its Director of Mental Health, and teaching social welfare policy. He had just become host of a public affairs program and I became his part-time research assistant. I was thrilled to work with him. He supported the merger of my two sides, the social worker and the photographer. He encouraged me to submit a photo to the Western Gerontological Society—now the American Society on Aging—for a photo contest. I won first prize for an intergenerational photo taken at The Elvirita Lewis Foundation (ELF) child care center in Santa Cruz, California. The next year, I won first prize for Three Generations of Women.
In the early 1980s, I directed an adult day health program for people who were chronically psychotic, i.e. schizophrenic or bipolar. Our clients were the survivors of institutionalization in the ‘60s and ‘70s. All had had serious chronic psychiatric problems. For the first time in a long time, they found themselves living in the larger community again. They and their families were ill equipped to cope. Most came to our program five days a week mainly so that their families could have respite.
I once asked a geriatric psychiatrist what I could do that would help these disturbed older people. He simply answered, “Help them find peace.” We used the expressive therapies a lot in our programming—art, music, dance, photography. I had a great staff, we did our best, and I like to think we succeeded in some cases.
In a recent county-wide survey, Older Adult Needs Assessment: Determining Priorities (1/16), older adults listed two of their top six priority areas as ‘Losing my memory’ and ‘Feeling isolated or depressed’.
I’ve been frustrated in this work at times, because aging simply isn’t on anyone’s radar screen. We are dealing with three stigmas—aging, mental health and dementia—not too sexy. The truth appears to be that everyone wants to live a long life but no one wants to grow old. We understand what it’s like to be a teenager or someone with children, because we’ve been through those experiences. But we can’t understand aging if we haven’t been there yet.
What are the benefits of Mental Health programs?
The good news is that 80% of depression and anxiety cases are treatable! To alleviate depression, people need a supportive community, be it family or a faith or affinity-based community. Older adults need to have their personal care needs met. We must figure out what it looks like for people to age-in-place in a way that is healthy mentally as well as physically.
For information about mental health services, start by calling 415-457-INFO. Other great resources include:
BOOST (Behavioral Options to Optimize Senior Transitions) is a program at the Jewish Children and Family Services that offers outreach and in-home programs for older adults
NAMI (National Alliance on Mental Illness) provides information about ‘geriatric care managers’ who can help those families that can afford private care
HOPE and Senior Peer Counseling offer weekly supportive in-home counseling to counteract isolation
Another resource to understand Marin’s issues in mental health and older adults is the Grand Jury Reports:
2014-2015 Marin’s Mentally Ill
2013-2014 Aging in Marin: What’s the Plan?
Finally, I recommend the book How to Say It to Seniors by David Solie. He explains that older adults, like others, want control over their lives.
What are some innovations we can look forward to regarding mental health?
I dream of bringing PEARLS to our community. PEARLS (Program to Encourage Active Rewarding Lives for Seniors), is an evidenced-based in-home depression care management model for older adults who have minor depression or dysthymia and are receiving home-based social services from community agencies (such as Whistlestop’s Meals on Wheels).
Depression is not a normal part of growing older, and treatment works.
PEARLS is a brief, time-limited, participant-driven program that teaches depression management techniques to older adults with depression. It consists of eight 50-minute sessions of in-home counseling sessions provided by Depression Care Managers (social workers or mental health counselors) followed up by 3-6 telephone contacts over a 19 week period. My hope is that we can bring this program to Marin.
Tell us about your involvement with Aging Action Initiative (AAI): I first heard about AAI when I was a member of the Commission on Aging. At the time, there were two work groups starting to form, one for Mental Health and another for Dementia. The two workgroups ended up merging into one because our goals were similar. Our focus was on how to deal with challenging behaviors. We wanted to create a community program that would help people understand common challenging behaviors and connect with compassionate communication. The result was the Detect & Connect program (community workshops and a train the trainer course).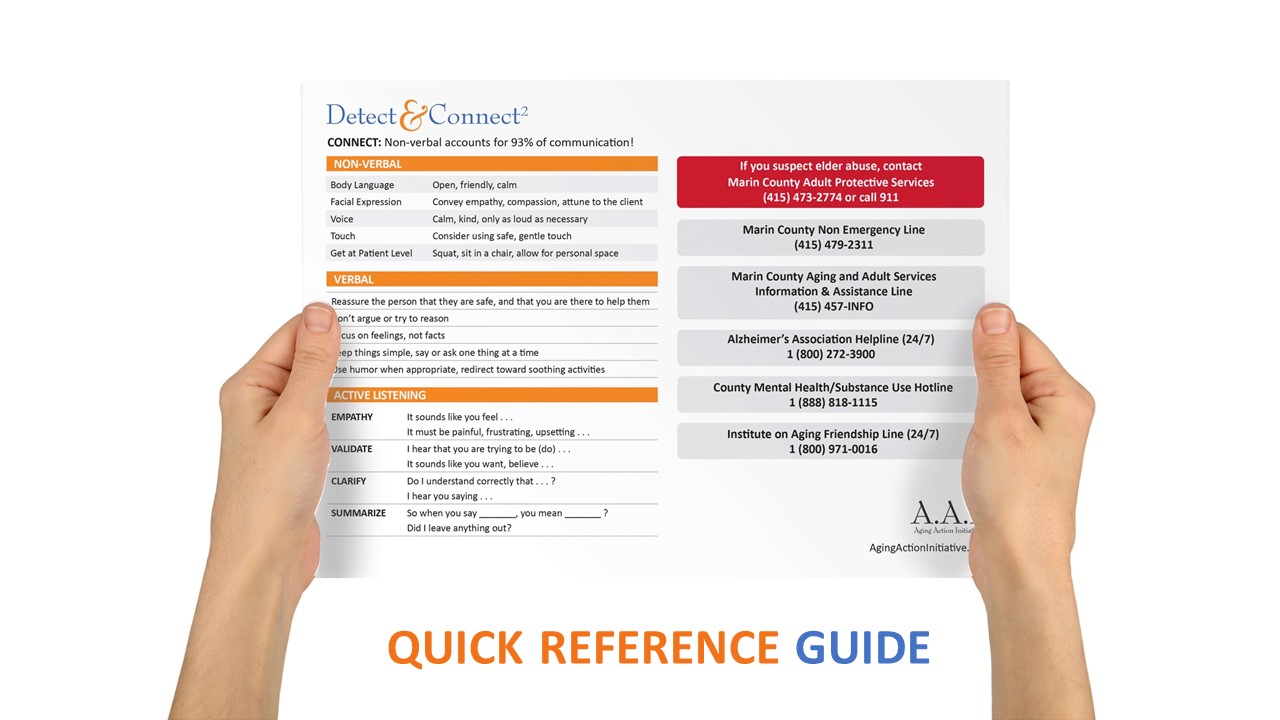
I volunteered to be part of the team that helped to create the Detect & Connect curriculum. We wanted something that would educate everyone—staff at Marin Housing, retirement communities, senior centers, bank tellers, neighbors, bus drivers—about how to approach an older adult with mental health issues, be they mood or cognitive. I believe we succeeded. My only wish is that the curriculum reaches a much larger pubic audience. I’m happy to hear that this program is continuing this year, with a training program for presenters this September, and the kickoff of the workshops in October.
Being part of the AAI Mental Health and Dementia work group was a wonderful collaborative experience. I have never seen that many colleagues in the same room with a shared common goal of working together to engage the community in the awareness of mental health problems—and the desire to provide services to meet the mental health challenges in Marin.
What is your vision of an age-friendly Marin?
All generations looking at concerns through, but not limited to, the lens of aging. We are learning! Age-friendly communities are proliferating throughout Marin.
Aging Action Initiative (AAI) is a collective effort of over 65 different agencies, grassroots organizations, commission and neighborhood groups, funded by the County of Marin and coordinated by MARINSPACE, collaborating for an age-friendly environment. For more information visit agingactioninitiative.org or connect with us on Facebook.





